"Recurrent miscarriage" is a diagnostic name that includes multiple pathological conditions.
The category is defined as any situation where live birth is not possible, repeated miscarriage, stillbirth, and early neonatal mortality before 22 weeks.
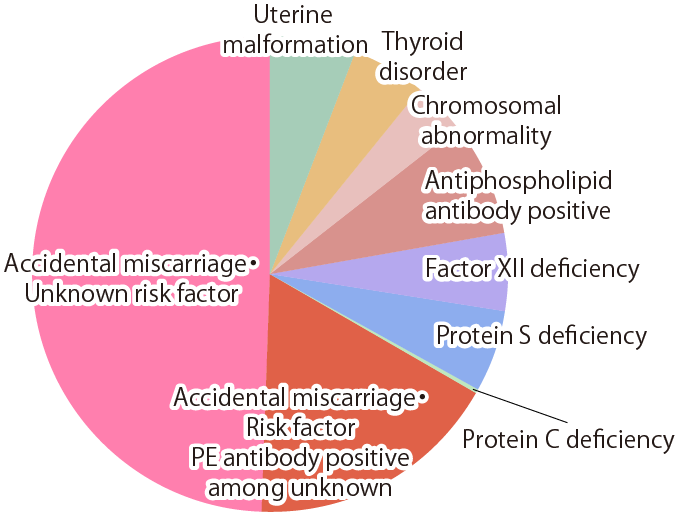
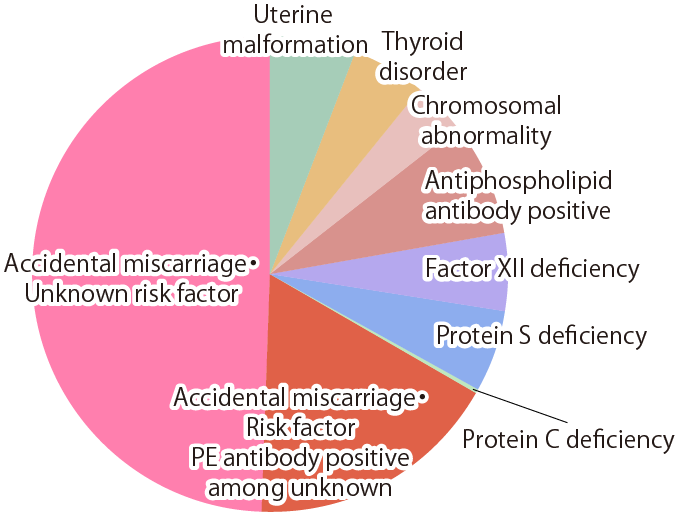
About half of these situations are incidental, and there is a high probability that the next pregnancy will proceed without any trouble, but the other half have abnormal conditions.
On examination, risk factors such as chromosomal abnormalities and uterine morphological abnormalities may be found.
- Spontaneous Abortion
This is defined as when the pregnancy ends unexpectedly after the gestational sac has been visualized.
- Customary Miscarriage
This is when a miscarriage occurs more than 3 times.
Stillbirths and neonatal mortality are not included.
- Recurrent Miscarriage
When a miscarriage occurs more than once.
Recently, this is a popular subject of study.
(Reference) Chemical Pregnancy
This is a miscarriage that occurs after a positive pregnancy test, but before the gestational sac is confirmed.
According to the Japanese Society Of Obstetrics & Gynecology, this is not included in miscarriage statistics.
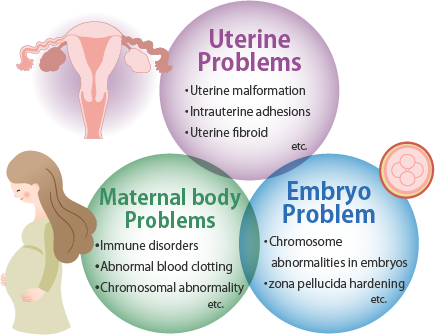
Causes of Recurrent Miscarriage
Causes of Recurrent Miscarriage
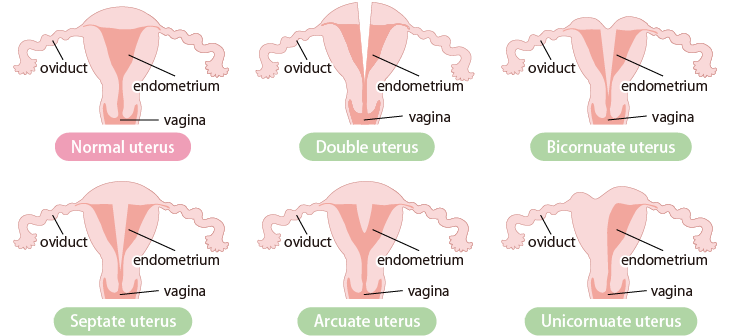
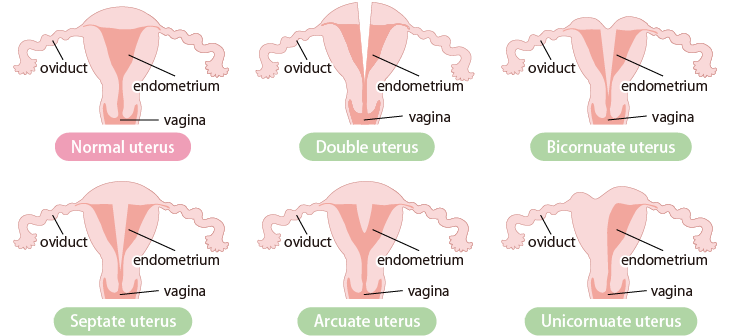
- Uterine Morphology
Uterine malformations are thought to affect implantation and fetal growth due to deformation of the uterine cavity (the space in which the fetus grows) and insufficient blood flow to the implantation site.
Main examples of uterine malformation
- Autoimmune disorders
It has been pointed out that excessive production of autoantibodies can easily cause blood clots in the endometrium of pregnancy and prevent angiogenesis, resulting in impaired pregnancy maintenance.
In particular, it has been pointed out that it is caused by antiphospholipid antibodies.
- Blood coagulation abnormality
Abnormal coagulation factors can easily cause blood clots in the placenta, leading to preterm birth.
- Allogeneic immune disorders
Half of the fetus’ genetic material is from the father, so it is halfway similar to a graft to the mother.
Immunological defense mechanisms work to establish pregnancy, and if this factor is out of balance, the fetus will be rejected as a foreign body, resulting in miscarriage.
- Chromosomal abnormalities of parents
If one or both parents have a chromosomal abnormality, it may cause defects in growth and subsequent miscarriage or implantation failure.
Repeated Implantation Failure
Even though there is no obvious cause, attempts to pregnant may not lead to pregnancy, including repeated embryo transfers.
In the case of unexplained infertility or recurrent implantation failure, there may be a chromosomal abnormality in the embryo or some abnormality in the patient.
In such cases, it is necessary to investigate.
Causes and Examinations for Repeated Implantation Failure
There are abnormalities in the uterine cavity, immune disorders, and vitamin and mineral abnormalities that are closely related to pregnancy.
IFCE (Implantation Failure Test)
In IFCE, we will check with a hysteroscope for abnormalities in the uterus (polyps, fibroids, adhesions, etc.) and chronic endometritis (micropolyps, redness, edema, etc.)
Allogeneic Immune Abnormality Test
One of the causes of recurrent implantation failure and recurrent miscarriage is abnormal functioning of the immune system.
In this abnormal situation, the immune system sees the embryo and fetus as foreign bodies and tries to eliminate them from the body (allogeneic immune abnormalities) resulting in abnormal pregnancy and discontinued pregnancy.
Tests for allogeneic immunological abnormalities include the following to check for any reaction from the body to eliminate transplanted embryos or fetus as foreign bodies.
- Peripheral Blood NK (Natural Killer) Activity
NK cells (natural killer cells) are involved in the immune tolerance needed to maintain pregnancy.
Excessive NK cell activity impairs the induction of angiogenesis and causes miscarriage by trying to eliminate the fetus as a foreign body.
Peripheral blood NK cell activity is often high in patients with infertility and recurrent miscarriage, and it patients who have experienced recurrent miscarriage may have levels significantly higher than those who have no history of miscarriage.
- Th 1 /Th 2
mmunity includes cell-mediated immunity and humoral immunity. Th 1 plays a central role in cell-mediated immunity, and Th 2 plays a central role in humoral immunity.
In recent years, Th 1 /Th 2 balance has been attracting attention as an immunological pregnancy maintenance mechanism.
Essentially, a pregnancy is maintained because Th 1 decreases and Th 2 increases.
One immunological cause of recurrent miscarriage may be autoantibodies such as antiphospholipid antibodies and mechanisms similar to the rejection of organ transplantation, both of which suggest that the Th 1 /Th 2 balance is disrupted.
If the balance is tilted too far toward Th 1 , the mother will recognize the fetus as a foreign body, causing rejection, implantation problems and miscarriage.
If you lean too much toward Th 2 , antibody production will become more active, and autoantibodies such as antiphospholipid antibodies will be produced, causing miscarriage.
The balance itself is important.
Blood Test of Substances Related to Pregnancy
This test will Judge whether the patient’s levels of substances (vitamin D, copper, zinc) that play an important role in the implantation environment and pregnancy are appropriate or need adjustment.
- Vitamin D
Vitamin D is best known for its role in calcium and bone metabolism, but it is also related to immunity, cancer, and allergies.
It has a very important role in pregnancy, and is related to the environment of the endometrium and implantation.
Women with higher vitamin D have a higher pregnancy rate for in vitro fertilization, and vitamin D deficiency increases the risk of early miscarriage.
In addition, it is said that the higher the blood vitamin D, the higher the AMH, that is, vitamin D deficiency leads to a decrease in ovarian reserve.
Vitamin D is taken from the diet and exposure to sunlight.
In recent years, vitamin D has become deficient in the general population due to reduced exposure to sunlight, making it extremely difficult to maintain sufficient levels with dietary intake alone.
Those who are reluctant to be exposed to sunlight should take supplements. (In food, it is abundant in herring, mackerel, sardines, tuna, shirasu, salmon, oocytes, mushrooms, etc.)
- Zinc / copper
Zinc is an important mineral for pregnancy.
Zinc promotes cell division in fertilized oocytes and regulates the environment in the uterus.
Copper, on the other hand, has the function of inhibiting implantation.
In other words, zinc deficiency allows more copper to be absorbed into the body, making implantation problems due to excess copper more likely.
In modern people's eating habits, retort pouch foods, frozen foods, processed foods such as snack foods, and vegetable-based diets make it harder to ingest zinc, which is abundant in meat and fish. Additives that are abundant in processed foods have the effect of inhibiting the absorption of zinc, and many people are zinc-deficient.
By supplementing zinc, the absorption of copper is suppressed, and it is possible to create a good environment for pregnancy.
Zinc is abundant in beef, pork, shellfish, crustaceans, peanuts and legumes.
Recurrent pregnancy loss and implantation failure test (blood test) at our hospital
| Recurrent Pregnancy Loss Test 1 |
Self‐pay ¥9,940
(With Tax: ¥10,934) |
- Anti cardiolipin antibody IgG (Anti CL antibody)
- Lupus anticoagulant (LAC) Russel’s viper venom
- Lupus anticoagulant (LAC) phospholipid neutralization test
|
| Recurrent Pregnancy Loss Test 2 |
Self‐pay ¥45,830
(With Tax: ¥50,413) |
- Anti cardiolipin antibody IgM (Anti CL antibody)
- Anti cardiolipin β 2 glycoproteinⅠcomplex antibody (Anti CLβ 2 GP 1 antibody)
- Anti‐phosphatidylserine prothrombin antibodies
- Anti‐phosphatidylethanolamine antibody Ig G (Anti PE antibody)
- FT 3
- FT 4
- TSH
- PT
- APTT
- Coagulant Ⅻ factor
- Protein C activity
- Protein S activity
|
| Recurrent Pregnancy Loss Test 3 |
Self‐pay ¥27,390
(With Tax: ¥30,129) |
- Th 1 /Th 2
- Natural Killer (NK) Activity
|
| Recurrent Pregnancy Loss Test 4 |
Self‐pay (for one person) ¥35,000
(With Tax: ¥38,500) |
- Chromosomal G‐banding method
|
| Recurrent Pregnancy Loss Test 5 |
Self‐pay ¥6,590
(With Tax: ¥7,249) |
|
| Recurrent Pregnancy Loss Test 6 |
With Tax: ¥43,750 |
|
Please note: The price including tax is listed based on the obligation to display the total amount.
Calculation errors may occur.
Some insurance may be applied. The final cost may differ.
If you have any questions, please ask the staff.
*Some tests might be covered by insurance.
Recurrent Pregnancy Loss Testing & Treatment
Based on the test results, we will select the treatment that corresponds to the abnormality.
Autoantibodies and coagulation abnormalities are treated with low-dose aspirin therapy *1 and heparin therapy *2
| Cause |
Test |
Treatment |
| Uterine form abnormalities |
- Hysterosalpingography(HSG)
- Transvaginal Ultrasound
- Hysterofiber(IFCE)
- Sonohysterography
|
Surgery based on the case |
| Endocrine abnormalities |
Thyroid function |
Blood test |
|
Screening by internal medicine doctor |
| Autoimmune abnormality |
- Anti cardiolipin antibody IgG,IgM
(Anti CL antibody)
|
Low-dosage Aspirin method(Until 28th week) *3
- If positive on the retest after the 12th week
Low-dosage Aspirin method continuation
(Until 28th week)
|
- Lupus anticoagulant(LAC)
- Anti cardiolipin β 2 glycoprotein I complex antibody(Anti CLβ 2 GP 1 antibody)
|
Low-dosage Aspirin method(Until 28th week) *3
- IF positive on the retest after the 12th week
Low-dosage Aspirin
(Until 28th week)
+
Heparin methods
(Until 36th week)
|
- Anti phosphatidylethanolamine antibody IgG(Anti PE antibody)
|
Low-dosage Aspirin method(Until 28th week)
However,in cases when the antibody value of negative kininogen is high,there is not need for treatment. |
- Anti-phosphatidylserine prothrombin antibodies IgG(Anit PS/PT antibody)
|
Low-dosage Aspirin method(Until 28th week) |
| Blood coagulation abnormalities |
|
- If extended
Low-dosage Aspirin method
|
|
- If deficient(under 60%)
Low-dosage Aspirin method(Until 28th week)
- If positive Anti PE antibody
Low-dosage Aspirin
(Until 28th week)
+
Heparin methods
(Until 36th week)
|
|
- If deficient(or over 30% to under 60%)
Low-dosage Aspirin method(until 28th week)
- If deficient(under 30%)
Low-dosage Aspirin
(Until 28th week)
+
Heparin methods
(Until 36th week)
However, if there is a miscarriage on or after the 10th week,
Low-dosage Aspirin
(Until 28th week)
+
Heparin methods
(Until 36th week) |
|
- If deficient(under 60%)
Low-dosage Aspirin methods(Until 28th week)
|
| Allogenic Immunity abnormalities |
|
- If 60% or over
Intralipid drip
|
|
- If 12 or over *4
Tacrolimus
|
| Parental chromosomal abnormalities |
- Chromosomal G-banding method
|
Genetic counseling |
| Vitamin/Mineral abnormalities |
|
Supplement |
*1)Low-dose aspirin therapy
Take 1 tablet of low-dose aspirin daily.
Duration: Start at the time of transplantation or in the middle of the high temperature period and continue to take until 28 weeks gestation.
Canceled if menstruation comes.
*2)Heparin therapy
Self-injection of 5000 units of heparin calcium once every 12 hours.
Period: Injection is started as soon as the fetal sac is confirmed.
Estimated price: 1 cylinder: ¥360 (with tax: ¥396) 1 day: ¥720(with tax: ¥792) 1 week: ¥5,040 (with tax: ¥5,544)
*A weekly blood test (liver function, platelets) will be performed within 1 month from the start of treatment.
[Blood test fee] ¥4,050(with tax: ¥4,455)
*A consent form is required for heparin therapy.
*A separate self-injection management fee of ¥2,000 (with tax: ¥2,200) is required at the start of heparin therapy.
*3)For those who are positive for antiphospholipid antibody syndrome, even if the retest is negative after 12 weeks, if there is a history of early miscarriage then
aspirin therapy + heparin therapy should be considered.
Example: Aspirin up to 28 weeks
Heparin up to 16 weeks
*4)When tacrolimus is used, the amount is adjusted individually.
*Others: In consideration of miscarriage history, age, etc., we may decide on treatment methods that differ from this page for individual customization.
*Inspection items: We will change the inspection items on a regular basis based on the latest data.
*Please note: The price including tax is listed based on the obligation to display the total amount. Differences in calculation may occur. The final cost may differ.
 |
 |
| About Implantation |
About Recurrent Miscarriage &
Implantation Failure |